Recovering from a heart event is a journey. Cardiac rehab at home helps adults in Sugar Land, Houston, and surrounding areas rebuild strength with nurse-led guidance—often starting within 24–48 hours of discharge, if your cardiologist approves. In addition, this option allows families to support loved ones without the stress of constant travel.
Definition: Cardiac rehab is a clinician-directed program of safe exercise, education, risk-factor control, and support. It restores heart health after events like heart attack or surgery, lowers readmissions, and improves quality of life.
- Get cardiologist clearance and check your home for safety.
- Set simple goals for vitals, symptoms, and activity minutes.
- Start light, guided activity with a nurse or therapist.
- Track medicines, BP/HR, symptoms, and progress daily.
- Advance your exercise and education week by week.
What is cardiac rehab?
Cardiac rehabilitation is a structured plan that blends step-by-step exercise, education (nutrition, medication use, and risk-factor control), and emotional support. At home, licensed clinicians work directly with your cardiology team. They monitor vitals, explain safe activity levels, and adjust goals as you improve. Therefore, it builds confidence while reducing risk of future events.
For patients who also need extra medical help, skilled home healthcare adds nursing, therapy, and monitoring for complex needs. This combined approach makes rehab safer and more effective.
Cardiac rehabilitation after open-heart surgery
After CABG or valve surgery, many people feel weak, sore, or afraid to move too much. At-home cardiac rehab uses gentle, safe activities like sternum-protective movements and breathing drills. Nurses guide pacing and incision care, while families learn red-flag signs. As a result, patients can progress steadily and avoid complications.
If your surgical wounds need special attention, in-home wound care helps prevent infection. This added support makes recovery smoother and more comfortable.
Can cardiac rehab be done at home?
Yes, it can. With cardiologist approval and basic safety checks, at-home rehab achieves similar results as clinic programs. Furthermore, it helps patients with transport issues, caregiver responsibilities, or comfort concerns. Regular visits, remote monitoring, and clear education provide accountability without leaving home.
To see how broader therapy works in a home setting, visit our page on in-home rehab services. These programs show how therapy adapts to each patient’s daily routine.
At-home cardiac rehab program: what to expect
- Assessment: A review of vitals, mobility, medicines, home safety, and goals.
- Plan: A clear weekly schedule for walks, strength, and balance work.
- Monitoring: Nurses check BP/HR, track symptoms, and confirm medicines.
- Education: Topics include diet, sleep, stress, smoking, and relapse prevention.
- Progression: Gradual increases in exercise with close oversight.
Cardiac rehab exercises at home: starter plan
Always follow your clinician’s advice. A typical “Week 1–2” plan might include:
- 3–5 short walks/day (3–10 minutes each), at a talking pace.
- Breathing drills (pursed-lip breathing) several times per day.
- Sit-to-stands from a sturdy chair, 1–2 sets of 5–10 reps.
- Gentle upper-body motions—sternum-safe after surgery.
- Daily logs for vitals and symptoms (dizziness, pain, swelling).
What qualifies me for cardiac rehab?
You may qualify if you recently had a heart attack, PCI/stent, CABG, valve surgery, angina, or certain cases of heart failure. Patients with a heart transplant or LVAD may also qualify. Finally, eligibility is confirmed by your cardiologist and insurance plan.
Real results from at-home care
Case 1 (6 weeks): After valve surgery, L. began with 5-minute walks. By week 6, she reached 25 minutes without fatigue. “Doing rehab at home made me consistent and calmer.”
Case 2 (8 weeks): Following a heart attack and stent, R. grew from light chair work to 30 minutes of brisk walking, 5 days per week. His labs improved and his confidence rose: “The check-ins kept me on track.”
For more evidence-based details, the CDC’s cardiac rehab resource explains national standards and proven benefits.
Disclaimer: This page is educational only. Always follow your clinician’s plan. If you have chest pain, severe shortness of breath, or concerning symptoms, call 911 right away.
Ready to begin?
Primary: Call Aleris Home Health to discuss cardiac rehab at home and confirm eligibility. Same-week starts are available in Sugar Land, Houston, and nearby areas.
Secondary: Want to learn more first? Download our “At-Home Cardiac Rehab Starter Guide” to see how goals, vitals, and pacing work together.
FAQs
How soon can I start cardiac rehab at home?
You can often start within 24–48 hours after discharge, if your cardiologist approves.
Do I need special equipment?
No. A BP cuff, scale, sturdy chair, and safe space for walking are usually enough.
How many days per week is the program?
Most patients begin with 4–6 days per week of short sessions, adjusting as they improve.
Is home cardiac rehab covered by insurance?
Coverage varies. Your care team can help check benefits, copays, and limits.
What symptoms should stop a session?
Stop for chest pain, severe shortness of breath, dizziness, or swelling. Call 911 for emergencies.
Can caregivers be involved?
Yes. They can help with scheduling, tracking vitals, and daily encouragement.
Will I still need clinic visits?
Yes. Home rehab complements, but does not replace, follow-ups and testing.
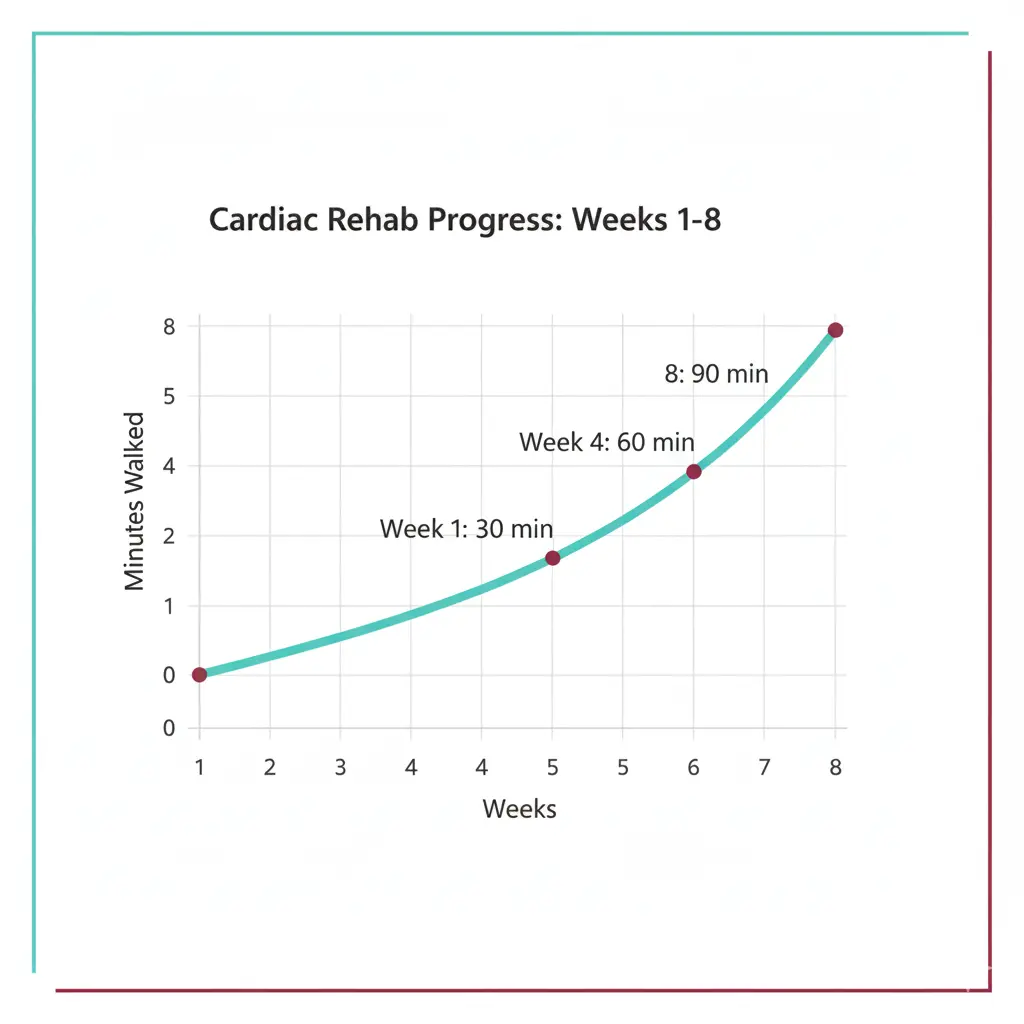
Line chart showing weekly walking minutes rising, with labels at weeks 1, 4, and 8.

